
“We are a high-quality, high-volume center,” said Grant Simons, MD, section chief, heart rhythm services at Englewood Hospital and Medical Center’s Heart and Vascular Institute. “We have the most advanced mapping and ablation technologies available. For example, we’re able to use 3-D mapping of atrial fibrillation to pinpoint problems in time and space with the clearest possible computer-rendered images.”
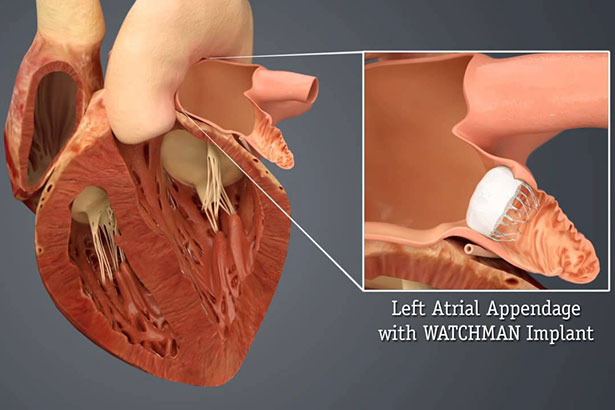
In fact, the reputation, experience and expertise of Dr. Simons and Englewood Hospital’s electrophysiology team were why the hospital was chosen as northern New Jersey’s first hospital to implant the WATCHMAN Left Atrial Appendage Device (Boston Scientific) for nonvalvular atrial fibrillation. The WATCHMAN device, which the FDA approved in 2015, is implanted into the heart’s left atrial appendage via a delivery catheter in the femoral vein to prevent blood clots from entering the bloodstream and causing ischemic stroke.
“While blood thinners can be effective, they have the potential for some dangerous side effects,” Dr. Simons said. “The WATCHMAN implant is actually a safer alternative to blood thinners, and it is more effective at reducing stroke risk among patients with atrial fibrillation. It also means a patient no longer needs to take blood thinners for the rest of his or her life.”
Although the relatively new procedure is only covered by insurance if a patient is considered an unsuitable candidate for long-term blood thinners, it is gaining traction. The procedure is relatively quick, taking anywhere from 45 minutes to 1.5 hours, and patients go home the next day requiring only a short-term course of anticoagulants.
Low Complications, High Innovations
“As awareness of the WATCHMAN increases, we’ve become a destination for this procedure and the LARIAT procedure, as well as cryoablation and mapping of atrial fibrillation,” Dr. Simons said. The LARIAT procedure is a minimally invasive alternative for patients with atrial fibrillation who are unable to take blood thinning medications. “We’re recommended because we have a very low complication rate, innovative technologies, a dedicated nurse practitioner program and a patient-centered system that quickly connects patients with physicians. We’ve eliminated that waiting-around, lost-in-the-system feeling,” Dr. Simons added.
In addition to the patient-oriented approach, the electrophysiology team works collaboratively, relying on decades of experience. “The team at Englewood is extremely experienced and that makes a huge difference when you’re working in such a complicated field,” said Asad Cheema, MD, medical director, electrophysiology laboratory who performs ablations for correcting arrhythmias at Englewood Hospital. “When you have a team of nurses and doctors that have been together for two decades, everything moves smoothly, everyone knows their roles, and everything runs like a well-oiled machine.”
Catheter ablation cures arrhythmias such as those seen in Wolff-Parkinson-White syndrome or atrioventricular nodal reentrant tachycardia, a type of supraventricular tachycardia. Dr. Cheema and the other physicians in the department often use radiofrequency energy to heat the catheter tip for precise ablation of live heart tissue. The procedure, which has a nearly 100% success rate, is quick and patients leave the same day, only needing to take a short course of aspirin.
Dr. Cheema explained that the laboratories at Englewood Hospital use the most advanced satellite sensors to pinpoint the exact location of catheters and the diseased tissue in the heart, allowing for cure of arrhythmias without risking side effects, such as esophageal damage. “All the latest technology and all the bells and whistles improve outcomes, recovery time and the patient’s prognosis,” he said. “It’s really a great way to treat patients.”
While heat cures arrhythmias, the electrophysiology team—which includes David Feigenblum, MD, PhD, Dmitry Nemirovsky, MD, and Satish Tiyyagura, MD—often also uses cryoablation to freeze heart tissue that causes paroxysmal atrial fibrillation. The surgeons use 3-D mapping to tailor the cryoballoon to variations in left atrial size and pulmonary vein anatomy.
The variety of expertise and experience creates a collaborative atmosphere at Englewood Hospital. “While we have our own teams, we often communicate and share thoughts on tough cases,” Dr. Cheema said. “We’re competing for excellence. We’re not competing against each other.”
Dr. Cheema sees something unique at Englewood Hospital. “We develop wonderful relationships because the hospital environment is friendly and patient oriented. Patients get directed to the right person very quickly.”
Posted September 2017
